D E L E G A T I O N
Delegation is the act of delegating. Good delegation “is a complex process in professional practice requiring sophisticated clinical judgement and final accountability for patient care” (Weydt, 2010), is essential in the management of Allied Health Assistants and can assist in making
the most of available resources to provide optimum patient care.
Although Allied Health Assistants (AHAs) may only implement programs that have been delegated to them by an Allied Health Professional
(AHP), AHPs find it hard to delegate a task or duty to an AHA for various reasons, some of them being:
·
* The AHP feels they can do a better job themselves, which may show a lack of confidence in the AHA’s abilities.
* The AHP believes the AHA does not have the appropriate skills, knowledge or experience required for the task to be delegated.
· * Delegating takes up too much precious time and the AHP feels they do not have enough time to delegate properly.
· * The AHP feels they should be able to do it ALL themselves without assistance
· * Doubtful of others to do the jobs as delegated.
* The AHP feels they do not have the skills to delegate well. ·
* The AHP assumes that the AHA is too busy and delegating a task to them will overwork them. ·
* The AHP prefers to work alone because it's less stressful. ·
* The AHP feels that it is easier to do it themselves than to ask an AHA ·
* The AHP fears losing control of valued activities when they are delegated to an AHA.
* Concern that others will see delegation as incompetence or laziness on the part of the AHP. ·
* A genuine fear that the AHA will take over the AHP’s job. ·
* Delegation is risky and risk taking is not encouraged in the organisation.
To have a good understanding of the delegation process there has to be a good perception of the key terms associated with this practice.
In their resource ‘Delegation, Monitoring and Evaluation of Allied Health Assistants’ Bell et all (2010, p.3) define three key terms:
the most of available resources to provide optimum patient care.
Although Allied Health Assistants (AHAs) may only implement programs that have been delegated to them by an Allied Health Professional
(AHP), AHPs find it hard to delegate a task or duty to an AHA for various reasons, some of them being:
·
* The AHP feels they can do a better job themselves, which may show a lack of confidence in the AHA’s abilities.
* The AHP believes the AHA does not have the appropriate skills, knowledge or experience required for the task to be delegated.
· * Delegating takes up too much precious time and the AHP feels they do not have enough time to delegate properly.
· * The AHP feels they should be able to do it ALL themselves without assistance
· * Doubtful of others to do the jobs as delegated.
* The AHP feels they do not have the skills to delegate well. ·
* The AHP assumes that the AHA is too busy and delegating a task to them will overwork them. ·
* The AHP prefers to work alone because it's less stressful. ·
* The AHP feels that it is easier to do it themselves than to ask an AHA ·
* The AHP fears losing control of valued activities when they are delegated to an AHA.
* Concern that others will see delegation as incompetence or laziness on the part of the AHP. ·
* A genuine fear that the AHA will take over the AHP’s job. ·
* Delegation is risky and risk taking is not encouraged in the organisation.
To have a good understanding of the delegation process there has to be a good perception of the key terms associated with this practice.
In their resource ‘Delegation, Monitoring and Evaluation of Allied Health Assistants’ Bell et all (2010, p.3) define three key terms:
|
Delegation
the process by which an AHP delegates activities to an AHA with appropriate education, knowledge and skills to undertake the activity safely. |
Monitoring
an on-going process of revieiwing an activity delegated by an AHP to an AHA to ensure set standards or requirements are being met. |
Supervision
a monitoring strategy where an AHP (directly) observes the competency of an AHA performing a delegated activity; their performance of an activity in different context (e.g.different clients) and; for the purpose of developing the AHA skills and competence. |

A good delegation process by an AHP includes matching AHA’s skills with the needs of the patient and the patient’s family to be able to provide effective patient-centred care. It is matching the right AHA skills to the task at hand which is often seen as the difference between delegating and assigning. According to Weydt (2010) “in the delegation process accountability rests within the decision to delegate, while the responsibility rests within the performance of the task”, and the AHP is accountable to follow up with the AHA to review the outcome of the delegated task. Occasionally the decision to delegate a task or duty is based on the tasks described in the AHA’s job description. This then involves assigning a task rather than delegating a task to an AHA.
The Framework (The Workforce, 2012) states it is anticipated that a”healthy dialogue” between AHPs and AHAs will take place to discuss “how to work effectively together in delivering high-quality patient care” and “a commitment among team members to work collaboratively”. For effective patient-centred care to be implemented all team members must “have a clear understanding of how their own position and the position of other team members contribute to the achievement of the team goals”.
The Framework (The Workforce, 2012) states it is anticipated that a”healthy dialogue” between AHPs and AHAs will take place to discuss “how to work effectively together in delivering high-quality patient care” and “a commitment among team members to work collaboratively”. For effective patient-centred care to be implemented all team members must “have a clear understanding of how their own position and the position of other team members contribute to the achievement of the team goals”.
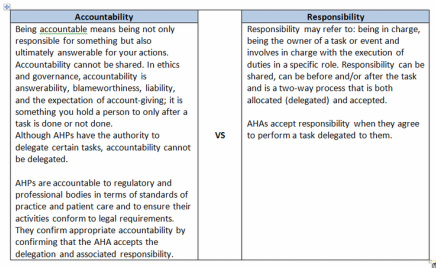 Accountability VS Responsibility
Accountability VS Responsibility
Accountability VS Responsibility
According to the Framework (The Workforce, 2012. p.24):
AHPs are accountable for delegating tasks and have a legal responsibility to determine that the AHA has the knowledge
and skill level required to perform the delegated task, provide an appropriate level of supervision and feedback, and to only delegate tasks that fall within the guidelines and protocols of the workplace.
AHAs are accountable for accepting the delegated task, as well as being responsible for their actions in carrying out the delegated task when they have the skills, knowledge and judgement to perform the delegation, the delegation is within the guidelines and protocols of
the workplace, and the AHA has an appropriate level of supervision and feedback.
According to the Framework (The Workforce, 2012. p.24):
AHPs are accountable for delegating tasks and have a legal responsibility to determine that the AHA has the knowledge
and skill level required to perform the delegated task, provide an appropriate level of supervision and feedback, and to only delegate tasks that fall within the guidelines and protocols of the workplace.
AHAs are accountable for accepting the delegated task, as well as being responsible for their actions in carrying out the delegated task when they have the skills, knowledge and judgement to perform the delegation, the delegation is within the guidelines and protocols of
the workplace, and the AHA has an appropriate level of supervision and feedback.
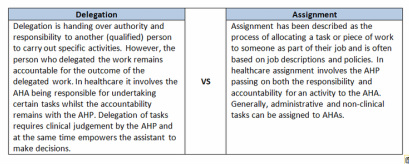 Delegation VS Assignment
Delegation VS Assignment
Assigning
Assigning a task to an AHA means to give the AHA a task or duty to do and transferring responsibility and accountability for that task or duty to the AHA. When assigning a task, such as with administrative or non-clinical task, besides providing appropriate familiarisation in undertaking the task if required, a few guidelines need to be kept in mind to:
·
* Provide guidance on how the AHA should undertake the task
* Provide parameters within which the AHA can make decisions ·
* Ensure the AHA knows when they should seek advice from their supervisor
The consent of the AHA contracting the task or duty is not necessary in an assignment. In contrast, in delegation, the AHA to whom the task is transferred must accept that authority and responsibility.
Assigning a task to an AHA means to give the AHA a task or duty to do and transferring responsibility and accountability for that task or duty to the AHA. When assigning a task, such as with administrative or non-clinical task, besides providing appropriate familiarisation in undertaking the task if required, a few guidelines need to be kept in mind to:
·
* Provide guidance on how the AHA should undertake the task
* Provide parameters within which the AHA can make decisions ·
* Ensure the AHA knows when they should seek advice from their supervisor
The consent of the AHA contracting the task or duty is not necessary in an assignment. In contrast, in delegation, the AHA to whom the task is transferred must accept that authority and responsibility.
Principles of effective delegation
Delegation is situation based and as such depends on the complexity of the task at hand, the risk involved if the task cannot be completed as required as well as the commitment and competence of the team members.
In delegating a task or duty, AHPs should have regard for the following principles:
1. The primary motivation for delegation should be to serve the interests of the patient and as such the decision to delegate a task or duty should be based on the needs of the patient. Consent should be sought from the patient in question if the task involves a client specific activity.
2. Diagnosis and clinical management and treatment plans are established by AHPs and these should not be delegated to AHAs.
3. AHPs should not delegate tasks and responsibilities beyond their own level of skill and experience.
4. AHPs should determine whether it is appropriate to delegate a task to an AHA, the complexity of the task needs to be considered, and only delegate if it is appropriate. Also, the level of experience held by the AHA and the complexity and risk associated with the delegated task will define the level of instruction specification that should be guided by the AHP.
5. The skills and competency of the AHA accepting the delegation needs to be considered meaning that the AHA to whom task is being delegated must have the level of experience and skills to perform the task safely and within their scope of practice.
6. Delegating is not the same as ‘dumping’ or‘imposing’ tasks on the AHA. It should be a two-way communication and as such good verbal communication skills by both the AHP and AHA are necessary. Once the required elements of the task have been evaluated by the AHP, the task being delegated should be discussed and, if both the AHP and AHA feel confident, then the AHA can carry out the delegated task. If the AHA does not feel confident undertaking the task, then this need to be communicated and the appropriate knowledge, skills and confidence should be acquired before the task is
delegated.
7. In delegating a task, AHPs should provide clear outlines of the details of the task and all necessary information through:
(a) clear instructions on the outcomes to be achieved
(b) clear processes to be followed in undertaking the task
(c) guidance on how to manage any perceived risks
(d) alternative strategies to be utilised if modification is required
(e) clear guidance on when further advice or direction should be sought from the AHP.
8. The level of supervision and feedback provided to an AHA should be appropriate, having regard for the knowledge and skill level of the AHA, the needs of the patient, the service setting and the task assigned.
9. AHAs have responsibility for raising any issues related to undertaking the delegated task, and should request additional information and/or support as required.
10. AHAs should be aware of the extent of their expertise at all times and seek support from AHPs
Delegation is situation based and as such depends on the complexity of the task at hand, the risk involved if the task cannot be completed as required as well as the commitment and competence of the team members.
In delegating a task or duty, AHPs should have regard for the following principles:
1. The primary motivation for delegation should be to serve the interests of the patient and as such the decision to delegate a task or duty should be based on the needs of the patient. Consent should be sought from the patient in question if the task involves a client specific activity.
2. Diagnosis and clinical management and treatment plans are established by AHPs and these should not be delegated to AHAs.
3. AHPs should not delegate tasks and responsibilities beyond their own level of skill and experience.
4. AHPs should determine whether it is appropriate to delegate a task to an AHA, the complexity of the task needs to be considered, and only delegate if it is appropriate. Also, the level of experience held by the AHA and the complexity and risk associated with the delegated task will define the level of instruction specification that should be guided by the AHP.
5. The skills and competency of the AHA accepting the delegation needs to be considered meaning that the AHA to whom task is being delegated must have the level of experience and skills to perform the task safely and within their scope of practice.
6. Delegating is not the same as ‘dumping’ or‘imposing’ tasks on the AHA. It should be a two-way communication and as such good verbal communication skills by both the AHP and AHA are necessary. Once the required elements of the task have been evaluated by the AHP, the task being delegated should be discussed and, if both the AHP and AHA feel confident, then the AHA can carry out the delegated task. If the AHA does not feel confident undertaking the task, then this need to be communicated and the appropriate knowledge, skills and confidence should be acquired before the task is
delegated.
7. In delegating a task, AHPs should provide clear outlines of the details of the task and all necessary information through:
(a) clear instructions on the outcomes to be achieved
(b) clear processes to be followed in undertaking the task
(c) guidance on how to manage any perceived risks
(d) alternative strategies to be utilised if modification is required
(e) clear guidance on when further advice or direction should be sought from the AHP.
8. The level of supervision and feedback provided to an AHA should be appropriate, having regard for the knowledge and skill level of the AHA, the needs of the patient, the service setting and the task assigned.
9. AHAs have responsibility for raising any issues related to undertaking the delegated task, and should request additional information and/or support as required.
10. AHAs should be aware of the extent of their expertise at all times and seek support from AHPs
Activities that could be considered for delegation:
• Activities that are frequently performed
• Activities that are performed using an established sequence of steps
• Activities that do not require complex use of AHP judgment
• Activities which have predictable results and minimal risks
Some final thoughts about delegation:
- When delegating a task, ask yourself the question if the delegation is ‘task based’ rather than ‘judgment based’.
- Delegation is a skill that requires knowledge and practice and is influenced by a good interpersonal relationship between the AHP and the AHA.
- Delegating a task requires the AHP to use critical thinking skills in order to match staff expertise with patient and family needs.
- Delegation is based on knowledge and trust in each other’s capabilities, respect, and an understanding of professional practice which often happens when AHPs and AHAs consistently “partner up” with each other. This can lead to more effective delegation processes and the confidence by both the AHP and AHA that complex tasks and duties can be accomplished.
- Delegation is the “invitation to participation”(Weydt, 2010) and as such can be considered a four-step process and is as simple as
CAAP:
• Activities that are frequently performed
• Activities that are performed using an established sequence of steps
• Activities that do not require complex use of AHP judgment
• Activities which have predictable results and minimal risks
Some final thoughts about delegation:
- When delegating a task, ask yourself the question if the delegation is ‘task based’ rather than ‘judgment based’.
- Delegation is a skill that requires knowledge and practice and is influenced by a good interpersonal relationship between the AHP and the AHA.
- Delegating a task requires the AHP to use critical thinking skills in order to match staff expertise with patient and family needs.
- Delegation is based on knowledge and trust in each other’s capabilities, respect, and an understanding of professional practice which often happens when AHPs and AHAs consistently “partner up” with each other. This can lead to more effective delegation processes and the confidence by both the AHP and AHA that complex tasks and duties can be accomplished.
- Delegation is the “invitation to participation”(Weydt, 2010) and as such can be considered a four-step process and is as simple as
CAAP:
|
COMMUNICATE |
APPRECIATE |
ADVOCATE |
PARTICIPATE |
